Bone Marrow Transplantation in Medical Park Hospitals Group
A treatment program, providing both service and training at international standards, is offered in stem cell and bone marrow transplantations in adult and children at Bone Marrow Transplantation Departments within the scope of Medical Park Hospitals Group. Transplantation Programs include clinical research in high dose chemotherapy and long-term outcome for bone marrow transplantations. The Bone Marrow Transplantation Multidisciplinary Team is comprised of physicians, nurses, pharmacists, therapists, social workers and administrators specializing in all aspects of stem cell transplantation. The Bone Marrow Transplantation Program is heavily supported by specialty programs based in the Divisions of Intensive Care Unit, Pulmonary Medicine, Infectious Diseases, Renal Medicine and other specialty services of the Medical Center.
We provide services for our patients with the aid of our team of experienced physicians at all our Bone Marrow Transplantation centers supported by a state of the art laboratory, and equipment and hardware that comply with international standards.
Our Bone Marrow Transplantation centers are certified by Ministry of Health and EBMT for conduct of autologous, allogeneic, matched-unrelated and reduced intensity transplantations. Our Units are also certified as Unrelated Donor Harvests by EBMT. At these centers, patient rooms and corridors are equipped with a HEPA Filtering system, which reduces the risk of airborne infections. The transplantation can be performed by using either the stem cells of the patient (autologous) or his/her siblings (allogenic) or if the patient does not have a sibling who is histocompatible, then the procedure can be conducted by using stem cells donated by people other than relatives to international bone marrow banks. Furthermore, cord blood transplantations, oriented by the in-vitro fertilization method, is one of the factors that differentiates us from others. Bone marrow transplantation decisions are taken in the Transplantation Council.
Autologous Bone Marrow Transplantation
It implies transplanting native stem cells, or in other words, own stem cells of the patient.
This type of transplantation is usually preferred for lymphomas, multiple myeloma (MM), germ cell tumors and acute leukemia –albeit rare.
Autologous stem cell transplantation: It is reserved for reinforcing outcomes of chemotherapy in patients with multiple myeloma or with some high-risk lymphomas. Autologous stem cell transplantation is preferred for recurrences of many lymphomas.
Prior to the autologous stem cell transplantation, your cardiac and respiratory functions are assessed and investigations are made regarding contraindications of transplantation.
When patient's own stem cell is collected, presence of diseased cells among stem cells is a risk that should be taken into account. Accordingly, when cryopreserved stem cells are re-transplanted to the patient, diseased cells that are possibly found among healthy stem cells may lead to recurrence.

Allogenic Bone Marrow Transplantation
This method implies transplanting stem cells that are collected from a fully compatible person – whether or not – to the patient.
Since all stem cells collected are intact, risks pertaining to autologous transplantation do not apply. In allogeneic transplantation, transplanting the immune system of healthy person is advantageous.
When stem cells of another person is transplanted, immune systems may not be completely compatible. Thus, immune system of the donor may react against recipient's organs. It may cause damage in liver, skin, bone marrow and intestines. This is referred as “graft versus host disease". This condition can be treated, but organ insufficiency may develop, as organ damage has already occurred. This risk does not apply to allogeneic transplantation.
Although allogeneic stem cell transplantation is more frequently performed for cancer patients, it can also be preferred in diseases that are characterized with bone marrow insufficiency.
Primary diseases that allogeneic stem cell transplantation is a therapeutic option:
Acute leukemia (acute myeloid leukemia, acute lymphoblastic leukemia)
Myelodysplastic Syndrome (MDS).
Severe aplastic anemia and other bone marrow insufficiency conditions (Fanconi anemia, Paroxysmal nocturnal hemoglobinuria, pure erythroid aplasia)
Non-Hodgkin lymphoma
Hodgkin lymphoma.
Chronic leukemia (chronic myeloid leukemia, chronic lymphocytic leukemia)
Haploidentic Bone Marrow Transplantation
In this type of transplantation, donor is a relative of patient who is not fully compatible.
It is a good alternative for patients who has no fully HLA-compatible donor. Fully compatible donor should be preferred, but if there is no such donor, partially compatible related donor should be considered. The consequence of this method in patients, who have not a chance to spend time searching for a non-related donor, is as successful as other transplantation methods. The most important disadvantage of haploidentical transplantation is higher risk of infection (since there is a significant antigen incompatibility). Therefore, it is necessary to monitor infections very carefully and take protective measures timely.
If a donor is searched for allogeneic stem cell transplantation, tissue groups of siblings, if available, are first analyzed. If no fully compatible donor can be found among siblings, close relatives of patient can be screened and final option will be “bone marrow banks", if screening result is negative. It may take 2 to 10 months to search for a compatible donor from bone marrow banks.
Patient is first given high-dose chemotherapy in allogeneic stem cell transplantation, similar to autologous stem cell transplantation. Next, stem cells collected from a healthy donor (sibling, related or non-related) are transplanted to the patient. These stem cells enable production of healthy blood cells in bone marrow of the patient.
In allogeneic stem cell transplantation, “Graft versus host disease"(GvHD) is a possible risk that is secondary to tissue incompatibility between donor and patient. GvHD is a serious disease that can cause severe damage in organs of recipient. Therefore, it is critically important that patient and donor are fully compatible to the maximum extent possible.
Bone marrow is responsible for synthesis of cells that are needed for life and for coping with harmful factors and results. Uncontrolled or false synthesis or inability to synthesize these cells may result with diseases.
After these diseases occur, hematopoetic stem cell transplantation can be sometimes required due to recurrence of disease, even if recoveries can be achieved with various medical therapies, and/or inability to achieve recovery or need to high-dose chemotherapy in order to achieve recovery.
One should always remember that in bone marrow transplantations, patients are vulnerable to infection and sometimes bleeding. Generally, almost all patients who undergo allogeneic transplantation use immunosuppressive drugs and thus, one should be very careful for both risks of infection and drug interactions in other therapies.
While these risks are highly possible in allogeneic transplantations, there are short-term risks in autologous transplantations as no immunosuppressive drug is used. The compliance between stem cell of donor and tissue of patient is ensured with various immunosuppressive therapies.
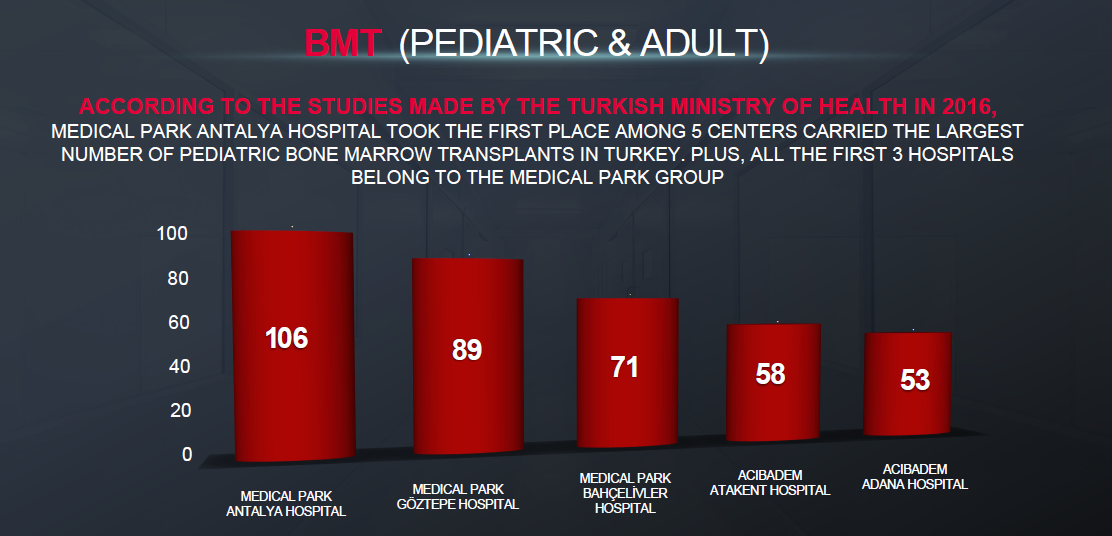
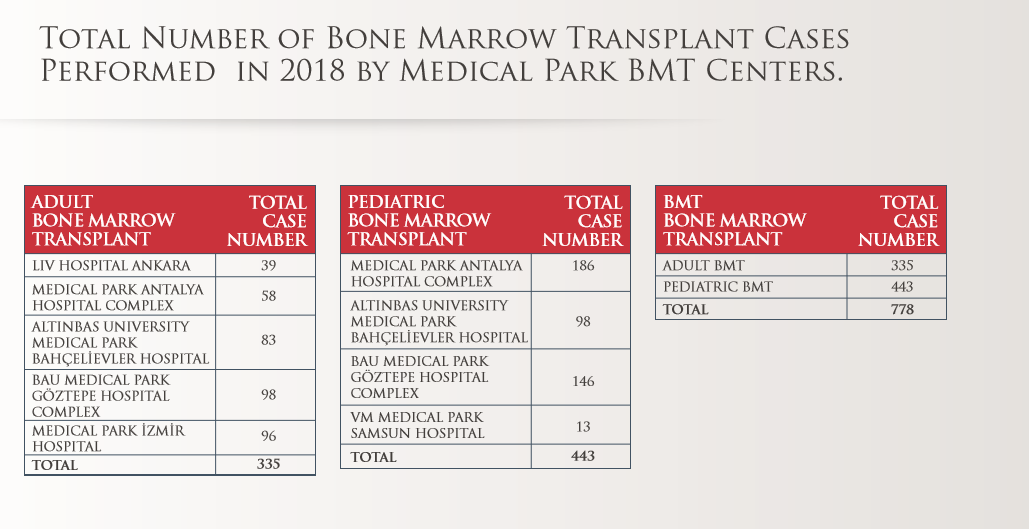
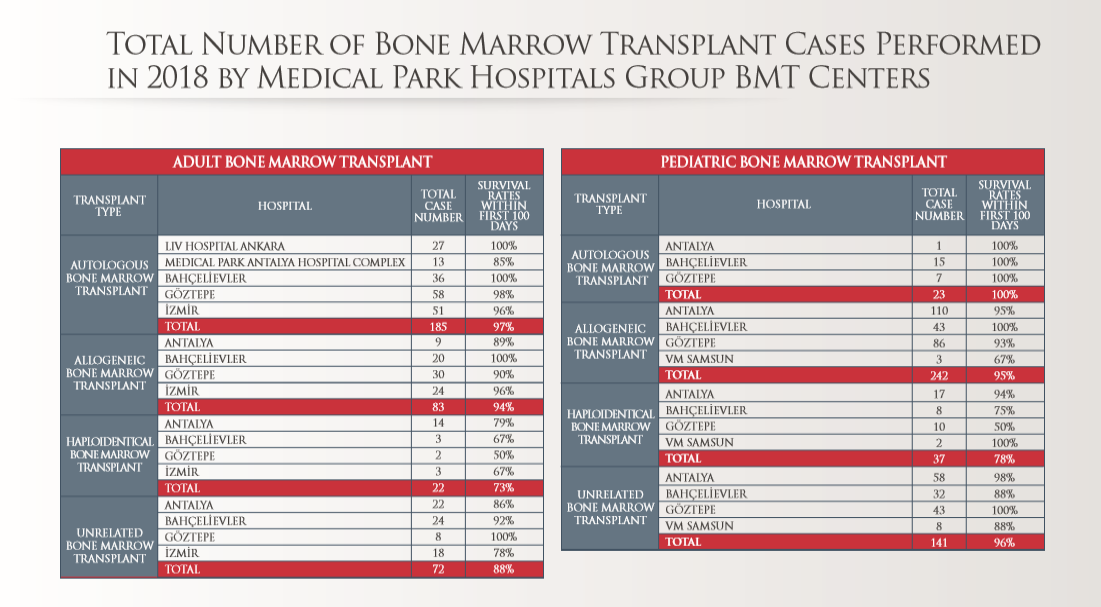
Adult Bone Marrow Transplant Centers
Medical Park Antalya Hospital Complex
Medical Park Göztepe Hospital Complex
Medical Park Bahçelievler Hospital
Medical Park İzmir Hospital
Pediatric Bone Marrow Transplant Centers
Medical Park Antalya Hospital Complex
Medical Park Göztepe Hospital Complex
Medical Park Bahçelievler Hospital
Medical Park Samsun Hospital
Bone Marrow Transplantation
For bone marrow transplantation, not only native stem cells of the patient are used, but also stem cells of another person can be transplanted, if particular criteria are met. Transplantations are categorized according to the source of stem cell.
How bone marrow is obtained for transplantation and how peripheral stem cells are collected for transplantation?
Stem cells to be used in transplantation can be collected from bone marrow, peripheral blood and umbilical cord blood of mothers who deliver recently. Although stem cells collected from peripheral blood are usually primarily preferred, stem cells collected from bone marrow will be preferred in benign diseases, such as aplastic anemia, thalassemia and immune deficiency syndromes.
Peripheral stem cell is harvested with apheresis device after cytokines, which help stem cells in bone marrow migrate to peripheral blood and are referred as granulocyte colony stimulant factor (G-CSF), are used.
For patients in need of autologous transplantation, stem cells can be harvested from peripheral blood using G-CSF following chemotherapy, while leukocyte count elevates.
Stem cell cannot be collected with these methods from patients whose bone marrow is extremely poor due to particular reasons. For these patients, stem cells can be collected from peripheral blood using strong stem cell stimulating preparations, which contain plerifaxor as active ingredient, concomitantly with G-CSF. Stem cells are collected from bone marrow, particularly in pelvic bone, using special needles under general anesthesia at operating room.
What should one expected in recovery process following transplantation?
Prior to allogeneic transplantations, patients generally receive high-dose chemotherapy drugs and immunosuppressive medications. Next, stem cells are transferred to patient via a central catheter. Risk of infection is high due to chemotherapeutic agents and immunosuppressive medications.
In this high-risk baseline period, such therapies should be given at bone marrow transplantation units that are equipped with hepafilter and ventilation systems which can clean infectious agents in the environment.
Even if those conditions are fulfilled, risk of infection is always high for those patients. Those patient should be closely monitored and treatment should be immediately started, if infection develops. After bone marrow of the donor settles in, it is possible to witness a fight between donor cells and tissues of patient. Immunosuppressive agents are used in these patients to avoid this condition. Successful outcome in those patients depends on the type of disease, stage of disease and degree of compliance between donor and patient.
Although bone marrow transplantation is a lifesaving option in diseases that originate from bone marrow and cannot be managed with medical treatments, the most important problem that a compatible sibling is not always available. In such cases, valuable options include non-related donors and donation of one tube of blood to bone marrow banks by volunteer donors.
To the contrary of organ donations, donation of bone marrow does not cause a deficiency in any organ or human body and this short-lasting procedure that causes a very honorable loss of time may save life of another person. At this point, anyone aged 18 to 55 can be a bone marrow donor. It is extremely necessary to increases awareness on this issue.
These transplantations can be in the form of autologous transplant - native cells of the patient are transplanted back to patient following high-dose medical therapies - or allogeneic transplantation – stem cells or bone marrow of another person are transplanted to patient.
Compatible siblings and related ones or tissue compatible non-related persons are possible donors for allogeneic transplantations. Stem cells derived from peripheral blood, bone marrow or umbilical cord blood can be used.
When is bone marrow (stem cell) transplantation necessary?
Bone marrow cannot produce healthy blood cells due to diseases that influence the bone marrow, such as leukemia or myelodysplastic syndrome;
Bone marrow cannot provide the immune system with sufficiently active cells or sufficient amount of hematopoietic cells in conditions such as aplastic anemia;
Further sophisticated therapies are required for some diseases, such as myeloma, lymphoma, testicular cancer, neuroblastoma and medulloblastoma.
Congenital severe immune system deficiencies and some metabolic diseases.
Bone marrow transplantation plays a significant role also in congenital blood diseases. Bone marrow transplantation is the only therapeutic modality in thalassemia, sickle cell anemia and some rare blood related diseases.
Bone marrow transplantation is the single choice in conditions that are unresponsive to therapy or recurrent, especially in Non-Hodgkin lymphoma which is also seen in childhood. In recurrence of Hodgkin lymphoma - another form of lymph node cancer-, the same therapy method is applied.
Apart from these, it is known that stem cell and bone marrow transplantations both increase treatment-related risks and facilitates healing.
What are eligibility criteria for bone marrow transplantation?
First, HLA tissue compatibility should be ensured to transplant bone marrow. Full compatibility between patient and donor and incompatibility in maximum one tissue group are acceptable for bone marrow transplantation. Recently, transplantations with >50% compliance between related donors and patient can be performed, if there is no related or unrelated donor for the high-risk patient.
Is it possible that bone marrow is rejected by body during the transplantation?
If bone marrow does not start producing blood cells within first two weeks after transplantation, rejection of donor's bone marrow by the recipient is a risk. This rate varies from 5% to 12% in allogeneic transplantations depending on type of donor and compatibility. This problem is almost never faced in autologous transplantations.
Is recurrence possible after transplantation?
Recurrence after transplantation is a possible outcome. These possibilities vary depending on underlying disease.

